Sun, Sunscreens, and Skin Cancer – the Missing Link
Author: Jian Gao, PhD
Editor: Mr. Frederick Malphurs
Updated on January 1, 2024
Do Not Blame the Sun for the Skin Cancer Epidemic
Excessive sun exposure can indeed damage the DNA in the skin cells which could lead to cancer. However, let’s not miss the forest for the trees – as a survival necessity, our shirtless ancestors were in the sun hunting and gathering for millions of years, and farming for the last 10,000 years before the industrial revolution. If the sun caused so many skin cancers, humanity would have been wiped out long ago.
In fact, before the 1920s, skin cancer was rare. But since the 1940s, skin cancer incidence has skyrocketed up to 16-fold worldwide depending on the regions studied.1-4 On the other hand, during the same period, more and more people spent less and less time outdoors – working in workshops and offices.
In addition, if sun exposure is the main driver of the skin cancer epidemic, higher prevalence should have been observed in low-latitude regions with intensive solar radiation and vice versa. But that is not the case. According to World Cancer Research Fund International, all ten countries with the highest rate of melanoma (the deadliest skin cancer) except for Australia and New Zealand are in high latitude regions – Denmark, The Netherlands, Norway, Sweden, Switzerland, Germany, Slovenia, and Finland.
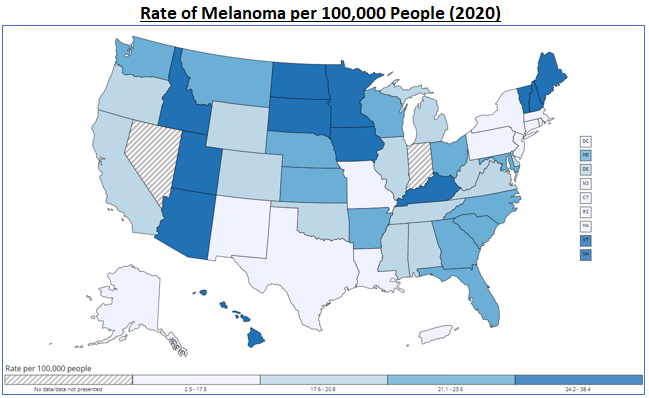
In the US, as shown in the map below (data source: CDC), except for Arizona, none of the states with high melanoma incidence (darker color) are in the Sun Belt.
Furthermore, the latest system review of literature conducted by researchers at Yale University in 2023 found the risk of melanoma is not higher among individuals with outdoor occupations.5
The thinning ozone layer above the earth, also called ozone depletion, may play some role in the increasing incidence of skin cancer, according to some researchers. But the skin cancer rate began to accelerate long before ozone depletion became an issue in the early 1980s. And the ozone depletion mainly affects the Antarctic region with little effect on the regions near the equator, but skin cancer cases in countries like Brazil near the equator have also shot up like other countries in the past decades.6 Even in other regions where UVB rays may have increased due to the thinning ozone layer, the increasing use of sunscreen should have more than fully countered the effect. In addition, the ozone layer only filters UVB, not UVA. In other words, the UVA level is not affected much by ozone depletion. And now the medical establishment believes melanoma is caused by UVA rather than UVB because the use of sunscreen has not made any dent on the soaring incidence of melanoma.
More intriguingly, in China, starting from the early 1990s and accelerating into the early 2000s, by 2019, the rate of melanoma (cases per 100,000 people) rose by more than 3-fold7 – the acceleration happened during a period when China was mostly covered by thick smog – not much UV light reached the ground. And indoor tanning was next to nonexistent in the same period.
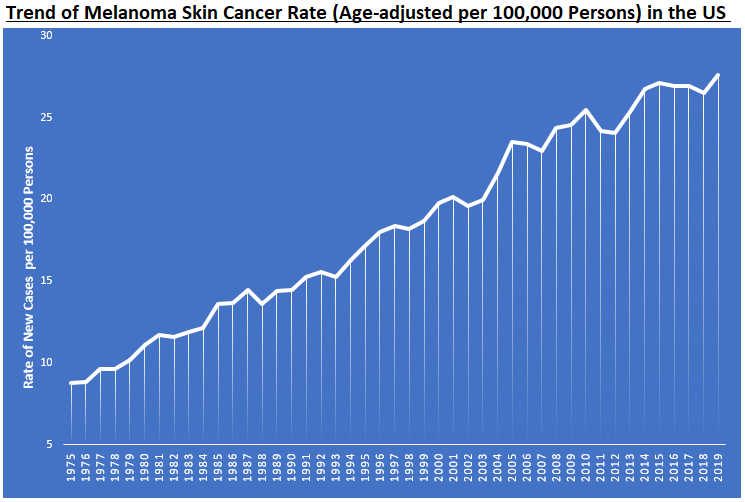
Tanning beds may have something to do with the rising of melanoma incidence since it increases UVB exposure. But Indoor tanning prevalence has decreased significantly over time – among all US adults, the percentage of users dropped from 10% in 2007 to 4% in 2018; among young adults aged 18 to 34, the users dropped from 14% to 4% in the same period.8 However, the incidence of melanoma keeps marching on as shown in the chart below (data source: the National Cancer Institute, NIH).9
In any event, let’s not ignore the big picture: since the 1920s, more and more people have spent less and less time in the sun because of rapid industrialization and the information revolution while the skin cancer incidence skyrocketed – do not blame the sun to which we owe our life for skin cancer.
What Drives the Skin Cancer Epidemic?
Australia, an elephant in the living room when it comes to skin cancer, has the highest rate of the disease in the world – a largely fair-skinned population loves outdoor activities in a country with plenty of sunshine. This can easily lead to a convenient conclusion: skin color and sun exposure is the culprit behind skin cancer. There is no doubt both skin tone and sun exposure play a role in developing skin cancer. But here is the inescapable question we must ask: why has Australia, like other regions such as Europe and North America, witnessed a continued drastic increase in skin cancer incidence (data source: Australian Government) and mortality rate (data source: study published in BMJ) as shown in the graphs below?
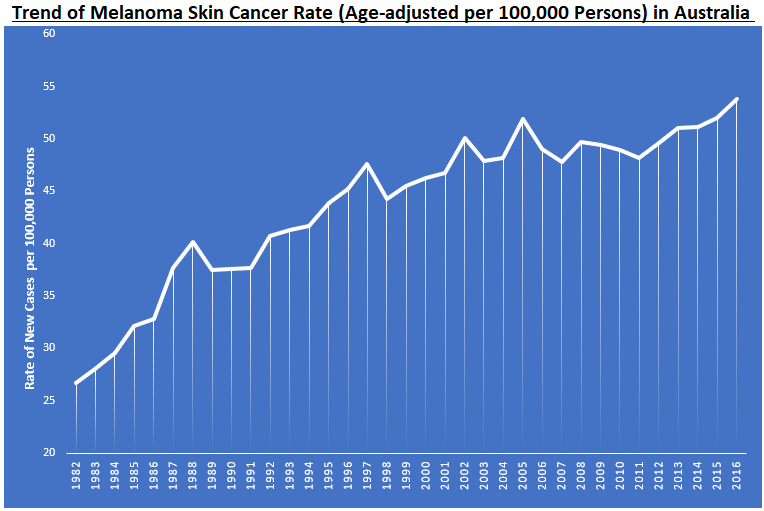
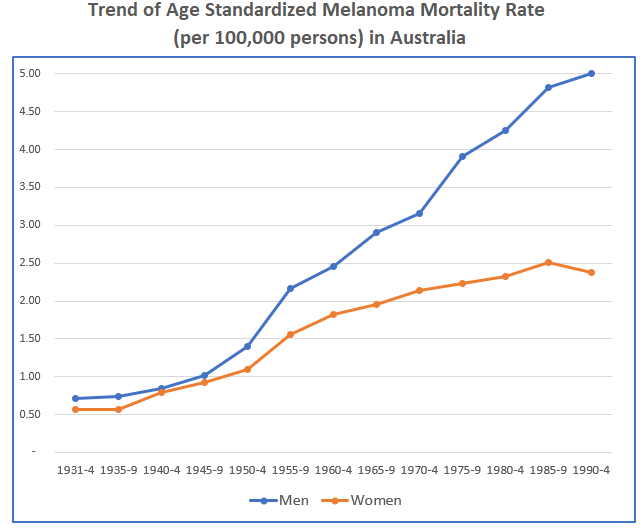
Obviously, it was not due to ozone depletion, which did not become a problem until the late 1970s or early 1980s while the rate of melanoma and mortality started to accelerate in the 1940s.10,11 In particular, the mortality rate for men (deaths per 100,000 persons) increased by 7-fold from the 1930s to 1990s in Australia despite continuously improved care designed to reduce mortality.
Better diagnosis and the change of diagnostic criteria might have played a role in the increase of melanoma incidence.12 But melanoma tends to metathesize rather than stay local. Therefore, it is unlikely that overdiagnoses were a significant driver behind the sharp rise of melanoma prevalence, which is substantiated by the skyrocketing melanoma mortality rate.
And tanning salons were not a significant contributor either – it was estimated that 281 new melanoma cases were attributable to indoor tanning in 2008 given tens of thousands new cases each year (indoor tanning has been highly regulated in Australia since 2015).13
So, what is behind the skyrocketing incidence and mortality of skin cancer since the 1940’s in Australia? Has the skin of Australians become fairer or had more sun exposure? Plus, worldwide, the populations with a high rate of skin cancer are largely in high latitude regions, and people working outdoors are not more likely to have melanoma compared to those working indoors. Something must be missing from the sun exposure and skin cancer equation.
For starters, there are three major types of skin cancer – basal cell carcinoma, squamous cell carcinoma, and melanoma. The first two types together are often called nonmelanoma skin cancer. Basal cells are found at the bottom of the epidermis (the outermost layer of the skin protecting our body from harm and keeping our body hydrated along with other functions). Basal cells produce new skin cells which push older cells toward the skin’s surface, where the old cells die and drop off. On the other hand, squamous cells, also called squamous epithelial cells, make up the middle and outer layers of the skin. Their major function is to act as a filter differentiating what can or cannot pass in or out of the skin. Because basal and squamous cells are in the outer layer of skin, they are more vulnerable to the sun’s UV rays.
Thankfully, both types of nonmelanoma skin cancer rarely spread and become lethal – surgery removal is almost always successful so long as the cancer is identified early. As a result, the governmental agencies do not even bother to collect data on nonmelanoma cancer anymore. So, there are no official counts of nonmelanoma cases in the US. But that does not mean the incident rate is not going up. According to the American Cancer Society , “about 5.4 million basal and squamous cell skin cancers are diagnosed each year in the US. … The number of these cancers has been increasing for many years.”
Melanoma skin cancer is a different story – it is less common compared to nonmelanoma skin cancer but often spreads to other parts of the body and becomes deadly. The American Cancer Society estimates that about 97,610 new melanomas will be diagnosed, and 7,990 individuals are expected to die from it in 2023. Melanoma starts in cells called melanocytes located in the bottom layer of the skin’s epidermis. Melanocytes produce melanin, a natural skin pigment, which gives skin its color and absorbs UV rays to protect skin cells from solar rays.
Despite the fact nearly everybody in the sun is soaked in sunscreen, melanoma incidence has continued to climb. Now, the new theory is melanoma is caused by UVA rather than UVB. But broad-spectrum sunscreen blocking both UVA and UVB was introduced in the late 1980s and early 1990s, yet the trend of melanoma prevalence has not budged. Do not forget most countries with high melanoma incident rate are in high latitude regions receiving much less UVA rays, and the rate of melanoma jumped more 300% in less than 30 years in China where very little sunshine was seen due to pollution. Plus, many studies have also found people working indoors are more likely to get melanoma than those working outdoors,5,14,15 and most melanomas appear on the parts of the body with little exposure to the sun.
All in all, the UVA theory does not add up – evidence and common sense tell us UVA is unlikely the main driver behind the skyrocketing melanoma prevalence, and broad-spectrum sunscreen is not likely to stop the relentless march of melanoma.
How can skin cancer, especially deadly melanoma, be stopped? The only way to bend the trend is to fix the root causes. And the first step is to understand what the root causes are. A good starting point is to understand why skin cancer was rare before the 1940s.
Before the 1940s, more people had more sun exposure compared with today. Why was the prevalence of skin cancer so low then? It is because nature gave the human body ingenious defense systems against damage from UV rays. The first defense system is the process of tanning. When exposed to UV rays from the sun, our skin produces melanin which darkens the skin and acts like an umbrella shielding our body from excessive solar bombardments.
Of course, melanin cannot block all UV rays, especially when sun exposure is excessive before the skin turns tan. Strong UV rays can indeed damage DNA in the skin cells. When that happens, the second defense system, i.e., repair, turns on. If the repair fails, the third defense system kicks in – programming the damaged cell to die, a process called apoptosis. Our body indeed has many troops holding the defense lines. For example, research has revealed the P53 gene, also called TP53, produces proteins that can repair damaged DNA and eliminate cells beyond repair.
It cannot be any clearer that the low skin cancer prevalence before the 1940s was due to the human body’s defense systems. Therefore, considering the following facts, the only logical explanation about the skyrocketing skin cancer incidence is the defense systems in our body have been compromised – the mechanisms preventing cancer from growing have stopped functioning properly.
- The number of skin cancer cases has been growing fast around the world for the last 80 years, happening mostly in developed and fast-growing countries, which has little correlation with ozone depletion either longitudinally or across populations.
- Skin cancer was rare before the 1940s while more people had much more sun exposure.
- Most countries with high skin cancer incidence are in the high latitude regions.
- The skin cancer rate more than tripled in less than three decades in China when blue sky was rarely seen due to heavy pollution.
- Indoor workers are more likely rather than less likely to get melanoma, which is also most likely to develop in parts of the body with little sun exposure.
- Tons of sunscreen has not made any dent on the soaring trend of skin cancer.
What has compromised our defense systems? The answer is plain and simple – the changing environment soaking us with toxic chemicals – nothing else has changed much as detailed in the article What’s behind the Soaring Chronic Diseases? Our body is poisoned by thousands of toxic chemicals in our food, drinking water, air, furniture, building materials, consumer products including cosmetics, cleaning agents, and even synthetic clothing.
No amount of sunscreen will stop skin cancer unless the root causes are addressed. According to the study published in JAMA dermatology in 2022, the number of newly diagnosed cases of melanoma will jump another 50%, deaths by 68% worldwide by 2040.16
Sunscreens May Do More Harm than Good
Riding on the soaring skin cancer cases, sunscreen sales rocketed in the US from $18 million in 1972 to $500 million in 1996, and then to an estimated $3.2 Billion in the year 2022.17,18 Worldwide, sun care product sales are forecasted to reach $18 Billion by 2027. So much so that sunscreen has become hazardous to the environment.
Since 2008 when researchers from Italy first identified the role of sunscreen ingredients causing coral bleaching in areas with high levels of human recreational activities,19 numerous studies have shown common ingredients in sunscreens pollute the ocean, bleaching coral reefs and threatening fish and other organisms that are essential for the ocean’s health.20 The US government agency National Oceanic and Atmospheric Administration states “Common chemicals used in thousands of products to protect against harmful effects of ultraviolet light threaten corals and other marine life.”21
Given the fact sunscreens damage corals and other marine life, it is hard to imagine they are benign to human health. In fact, the ingredients of common sunscreens can readily pass through the skin and get into the bloodstream. Upon confirming its earlier findings,22 in the second study published in JAMA in 2020, the FDA concluded “In this study conducted in a clinical pharmacology unit and examining sunscreen application among healthy participants, all 6 of the tested active ingredients administered in 4 different sunscreen formulations were systemically absorbed and had plasma concentrations that surpassed the FDA threshold for potentially waiving some of the additional safety studies for sunscreens.”23
Not so surprisingly, only two ingredients, zinc oxide and titanium dioxide, among the dozens used in different sunscreens, can be classified as safe – the health effects of others are unknown or downright harmful.24 For instance, independent labs found many sunscreens contain benzene, a known carcinogen or cancer maker.25
The most unsettling part is the unknowns – it is reckless to assume these sunscreen chemicals absorbed into our body are just innocent passersby going through urine to the toilet. Despite being an accepted principle in the judicial system, “presumption of Innocence until proven guilty” is downright dangerous in the chemical world. Few manmade chemicals are not harmful – evolution has not given our body enough time to learn to deal with them. They are either outright toxic or interrupt the normal functions of hormones and enzymes by occupying the receptors of the cells in our body.
In fact, in lab and animal models, many of these ingredients in sunscreens are shown to be endocrine disrupters, neurotoxic, and disrupting embryonic development.24,26-28 Of course, the findings of these ill effects in epidemiologic studies are inconsistent.29-30 This is not a surprise – sunscreen chemicals in the human body rarely reach the acute toxicity level, and chronic diseases including cancer are often a result of multiple chemicals or toxins working together.
It is dangerous to assume sunscreen is safe just because the direct link between sunscreen use and cancer or other disorders has not been firmly established. The chemicals in sunscreen may not be the chief culprit but could well be the last straw breaking the camel’s back – most often, it is the total toxic burden that makes the difference – our body uses the same enzymes to detoxify all the waste and poisons. In any event, these sunscreen chemicals seeping into the blood stream and thus every organ and tissue in our body cannot be good for our health. Those who are already having health issues or pregnant need to be more careful about sunscreen use.
Given all the unwanted detrimental effects, the irony is that studies have not found sunscreens effective in preventing skin cancer. A systematic review and meta-analysis published in European Journal of Dermatology in 2018 concluded “this systematic review does not confirm the expected protective benefits of sunscreen against skin cancer in the general population.” The ineffectiveness of sunscreens is obvious – skin cancer prevalence and sunscreen use have been growing in lockstep since the 1950s.
Are sunscreens a total sham? Probably not, but they must be used wisely. The benefit probably outweighs the harm when you would otherwise get sunburn unless sunscreen is applied – on occasions, for instance, before your skin gets tanned, for whatever reason (e.g., accompanying friends on the beach or playing a golf tournament) you ‘need’ to stay in the brutal sun for an extended period.
Keep in mind, skin tanning and sunburn are different. The former builds up your defense system to shield the UV rays, while the latter causes DNA damage.
So, sunscreen use is a tradeoff – on the one hand, it can prevent sunburn which could lead to cancer; on the other, it sends harmful (at least not beneficial) chemicals into the blood stream and thus every organ and tissue, which increases the total toxic burden of our body. Therefore, the use of sunscreen is a personal decision – we must be sunscreen smart. If you need to use sunscreen, read the EWG article explaining what ingredients to avoid.
No Reason to Be Heliophobic
Let’s not forget all living things on the planet owe their life to the sun – we humans are not an exception. Unfortunately, owing to the fear of skin cancer, too little rather than too much sun exposure has become a significant threat to our health.31-33 In particular, avoiding sun exposure and wearing sunscreens have led to widespread vitamin D deficiency, contributing to a myriad of maladies. Bear in mind, about 90% of the vitamin D our body needs is produced by the sun and our skin, and sunscreens block UVB rays and thus the synthesis of vitamin D.
There are hardly any diseases including melanoma not related to vitamin D deficiency or insufficiency.34-36 Vitamin D in fact is not a vitamin – it is really a hormone with receptors on each cell in our body (the only other hormone that has receptors on each cell of our body is the thyroid hormone). Vitamin D is as important if not more so than engine oil for your car, yet only one third of the population are vitamin D sufficient let alone in the optimal range.
According to the latest data from the National Health and Nutrition Examination Surveys (NHANES) published in 2022, the most authoritative data source on nutrition status, one in four or 25% of Americans are vitamin D deficient (<20 ng/mL), 41% are insufficient (20 -30 ng/mL), and only a little over one third (35%) are sufficient in vitamin D (>30 ng/mL).37 Among the 35% who are sufficient in vitamin D, probably half of them are not in the optimal range, although the exact percentage was not reported in the study.
Vitamin D deficiency or insufficiency can be easily corrected by taking dietary supplements. But the best way to raise the vitamin D level is through sun exposure, which not only produces vitamin D, but also several photoproducts which are beneficial to our physical and mental health.14 Of course, like many things in life, too much of a good thing can turn out to be bad – excessive sun exposure can wrinkle your face and even trigger skin cancer, which is now more true than before because of increased life expectancy and thus more accumulated sun exposure for aging populations.
When it comes to enjoying the sun, like all other things in life, moderation is the best of rules. To fully take advantage of the sun for your health, please read the book, The Vitamin D Solution, by Dr. Michael Holick, PhD, MD, the world’s foremost leading expert on sensible sun exposure and vitamin D.
About the Author and Editor: Jian Gao, PhD, is a healthcare analyst/researcher for the last 25 years who devoted his analytical skills to understanding health sciences and clinical evidence. Mr. Frederick Malphurs is a retired senior healthcare executive in charge of multiple hospitals for decades who dedicated his entire 37 years’ career to improving patient care. Neither of us takes pleasure in criticizing any individuals, groups, or organizations for the failed state of healthcare, but we share a common passion — to reduce unnecessary sufferings inflicted by the so-called chronic or incurable diseases on patients and their loved ones by analyzing and sharing information on root causes, effective treatments, and prevention.
Disclaimer: This article and any contents on this website are informational or educational only and should by no means be considered as a substitute for the advice of a qualified medical professional. It is the patients and caregivers’ solemn responsibility to work with qualified professionals to develop the best treatment plan. The author and editor assume no liability of any outcomes from any treatments or interventions.
References
- Hallberg O, Johansson O. Cancer trends during the 20th century. Journal of Australian College of Nutritional & Environmental Medicine Vol. 21 No. 1; April 2002: pages 3-8.
- Geller AC, Clapp RW, et al. Melanoma epidemic: an analysis of six decades of data from the Connecticut Tumor Registry. J Clin Oncol. 2013 Nov 20;31(33):4172-8. doi: 10.1200/JCO.2012.47.3728. Epub 2013 Sep 16. PMID: 24043747; PMCID: PMC3906570.
- Khatami M. Cancer; an induced disease of twentieth century! Induction of tolerance, increased entropy and ‘Dark Energy’: loss of biorhythms (Anabolism v. Catabolism). Clin Transl Med. 2018 Jul 2;7(1):20. doi: 10.1186/s40169-018-0193-6. PMID: 29961900; PMCID: PMC6026585.
- Helgadottir H, Isaksson K, Fritz I, et al. Multiple Primary Melanoma Incidence Trends Over Five Decades: A Nationwide Population-Based Study. J Natl Cancer Inst. 2021 Mar 1;113(3):318-328. doi: 10.1093/jnci/djaa088. PMID: 32577730; PMCID: PMC7936055.
- Maduka RC, Tai K, Gonsai R, et al. Indoor Versus Outdoor: Does Occupational Sunlight Exposure Increase Melanoma Risk? A Systematic Review. J Surg Res. 2023 Mar;283:274-281. doi: 10.1016/j.jss.2022.10.025. Epub 2022 Nov 21. PMID: 36423476.
- de Melo AC, Wainstein AJA, Buzaid AC, Thuler LCS. Melanoma signature in Brazil: epidemiology, incidence, mortality, and trend lessons from a continental mixed population country in the past 15 years. Melanoma Res. 2018 Dec;28(6):629-636.
- Bai R, Huang H, Li M, Chu M. Temporal Trends in the Incidence and Mortality of Skin Malignant Melanoma in China from 1990 to 2019. J Oncol. 2021 Aug 24;2021:9989824. doi: 10.1155/2021/9989824. PMID: 34475955; PMCID: PMC8407983.
- Bowers JM, Geller AC, Schofield E, Li Y, Hay JL. Indoor Tanning Trends Among US Adults, 2007-2018. Am J Public Health. 2020 Jun;110(6):823-828. doi: 10.2105/AJPH.2020.305605. Epub 2020 Apr 16. PMID: 32298165; PMCID: PMC7204456
- Cancer Stat Facts: Melanoma of the Skin. The Surveillance, Epidemiology, and End Results (SEER) Program, NCI, NIH. https://seer.cancer.gov/statfacts/html/melan.html
- Giles GG, Armstrong BK, Burton RC, et al. Has mortality from melanoma stopped rising in Australia? Analysis of trends between 1931 and 1994. BMJ. 1996 May 4;312(7039):1121-5. doi: 10.1136/bmj.312.7039.1121. PMID: 8620126; PMCID: PMC2350656.
- Erdmann F, Lortet-Tieulent J, Schüz J, et al. International trends in the incidence of malignant melanoma 1953-2008–are recent generations at higher or lower risk? Int J Cancer. 2013 Jan 15;132(2):385-400. doi: 10.1002/ijc.27616. Epub 2012 May 21. PMID: 22532371.
- Welch HG, Mazer BL, Adamson AS. The Rapid Rise in Cutaneous Melanoma Diagnoses. N Engl J Med. 2021 Jan 7;384(1):72-79.
- Gordon LG, Hirst NG, Gies PH, Green AC. What impact would effective solarium regulation have in Australia? Med J Aust. 2008 Oct 6;189(7):375-8. doi: 10.5694/j.1326-5377.2008.tb02082.x. PMID: 18837680.
- Garland FC, White MR, Garland CF, Shaw E, Gorham ED. Occupational sunlight exposure and melanoma in the U.S. Navy. Arch Environ Health. 1990 Sep-Oct;45(5):261-7
- Holick MF. The Vitamin D Solution. Hudson Street Press, a member of Penguin Group. 2010. New York, NY 10014.
- Arnold M, Singh D, Laversanne M, et al. Global Burden of Cutaneous Melanoma in 2020 and Projections to 2040. JAMA Dermatol. 2022 May 1;158(5):495-503. doi: 10.1001/jamadermatol.2022.0160. PMID: 35353115; PMCID: PMC8968696.
- https://www.motherjones.com/politics/1998/05/sunscam/
- https://www.globenewswire.com/en/news-release/2023/03/14/2626891/28124/en/Sun-Care-Products-Global-Market-to-Reach-23-2-Billion-by-2030-Innovations-Fuel-Growth-in-Suncare-ProductsMarket.html#:~:text=The%20Sun%20Care%20Products%20market,analysis%20period%202022%20to%202030.
- Danovaro R, Bongiorni L, Corinaldesi C, et al. Sunscreens cause coral bleaching by promoting viral infections. Environ Health Perspect. 2008;116(4):441–447. doi:10.1289/ehp.10966.
- Chatzigianni M, Pavlou P, Siamidi A, Vlachou M, Varvaresou A, Papageorgiou S. Environmental impacts due to the use of sunscreen products: a mini-review. Ecotoxicology. 2022 Nov;31(9):1331-1345. doi: 10.1007/s10646-022-02592-w. Epub 2022 Sep 29. PMID: 36173495; PMCID: PMC9652235.
- https://oceanservice.noaa.gov/news/sunscreen-corals.html
- Matta MK, Zusterzeel R, Pilli NR, et al. Effect of Sunscreen Application Under Maximal Use Conditions on Plasma Concentration of Sunscreen Active Ingredients: A Randomized Clinical Trial. JAMA. 2019 Jun 4;321(21):2082-2091.
- Matta MK, Florian J, Zusterzeel R, et al. Effect of Sunscreen Application on Plasma Concentration of Sunscreen Active Ingredients: A Randomized Clinical Trial. JAMA. 2020 Jan 21;323(3):256-267.
- The trouble with ingredients in sunscreens. EWG. https://www.ewg.org/sunscreen/report/the-trouble-with-sunscreen-chemicals/
- Nicole W. Skin Protection Dilemma: Testing Detects Benzene in Some Sun Care Products. Environ Health Perspect. 2022 May;130(5):54002. doi: 10.1289/EHP11423. Epub 2022 May 17. PMID: 35580036; PMCID: PMC9113541.
- Ruszkiewicz JA, Pinkas A, Ferrer B, et al. Neurotoxic effect of active ingredients in sunscreen products, a contemporary review. Toxicol Rep. 2017 May 27;4:245-259. doi: 10.1016/j.toxrep.2017.05.006. PMID: 28959646; PMCID: PMC5615097.
- Santander Ballestín S, Luesma Bartolomé MJ. Toxicity of Different Chemical Components in Sun Cream Filters and Their Impact on Human Health: A Review. Applied Sciences. 2023; 13(2):712. https://doi.org/10.3390/app13020712
- DiNardo JC, Downs CA. Can oxybenzone cause Hirschsprung’s disease? Reprod Toxicol. 2019 Jun;86:98-100. doi: 10.1016/j.reprotox.2019.02.014. Epub 2019 Mar 1. PMID: 30831214.
- Suh S, Pham C, Smith J, Mesinkovska NA. The banned sunscreen ingredients and their impact on human health: a systematic review. Int J Dermatol. 2020 Sep;59(9):1033-1042. doi: 10.1111/ijd.14824. Epub 2020 Feb 28. PMID: 32108942; PMCID: PMC7648445.
- Silva ESD, Tavares R, Paulitsch FDS, Zhang L. Use of sunscreen and risk of melanoma and non-melanoma skin cancer: a systematic review and meta-analysis. Eur J Dermatol. 2018 Apr 1;28(2):186-201. doi: 10.1684/ejd.2018.3251. PMID: 29620003.
- Mead MN. Benefits of sunlight: a bright spot for human health. Environ Health Perspect. 2008 Apr;116(4):A160-7.
- Alfredsson L, Armstrong BK, Butterfield DA, et al. Insufficient Sun Exposure Has Become a Real Public Health Problem. Int J Environ Res Public Health. 2020 Jul 13;17(14):5014. doi: 10.3390/ijerph17145014. PMID: 32668607; PMCID: PMC7400257.
- Holick MF. Sunlight, UV Radiation, Vitamin D, and Skin Cancer: How Much Sunlight Do We Need? Adv Exp Med Biol. 2020;1268:19-36.
- Muralidhar S, Filia A, Nsengimana J, et al. Vitamin D-VDR Signaling Inhibits Wnt/β-Catenin-Mediated Melanoma Progression and Promotes Antitumor Immunity. Cancer Res. 2019 Dec 1;79(23):5986-5998.
- Kanasuo E, Siiskonen H, Haimakainen S, et al. Regular use of vitamin D supplement is associated with fewer melanoma cases compared to non-use: a cross-sectional study in 498 adult subjects at risk of skin cancers. Melanoma Res. 2023 Apr 1;33(2):126-135.
- Heaney RP. Vitamin D in health and disease. Clin J Am Soc Nephrol. 2008 Sep;3(5):1535-41.
- Cui A, Xiao P, Ma Y, et al. Prevalence, trend, and predictor analyses of vitamin D deficiency in the US population, 2001-2018. Front Nutr. 2022 Oct 3;9:965376. doi: 10.3389/fnut.2022.965376. PMID: 36263304; PMCID: PMC9573946.
